Principles of UV + Ozone Disinfection

Principles of UV and Ozone Disinfection and the Risks of Floors and Shoes in Pathogen Dissemination
By: Robyn Collins
Robyn Collins, Vice President, PathO3Gen Solutions is a seasoned professional with more than 30 years experience at Fortune 500 companies and start-ups.
__
I think we can all agree that Sterile Processing and Operating Rooms should be the cleanest areas in the hospital, but why is cleanliness so important? The CDC estimates that in U.S. hospitals alone HAIs account for an estimated 99,000 preventable deaths each year, and cost the economy between $35 — $45 billion. In addition, the COVID-19 pandemic fueled a big jump in Healthcare-Associated Infections (HAIs). A CDC analysis published in September 2021 states that “significant increases in 2020 were observed for CLABSI, CAUTI, VAE, and MRSA bacteria compared to 2019. The largest increases occurred during the 4th quarter (October, November, December) of 2020. Researchers attributed the increase to various challenges related to the COVID-19 pandemic, including staffing shortages and high patient caseloads, which limited hospitals’ ability to follow standard infection control protocols. “The Intensive Care Units (ICU’s) experienced an even more significant impact. The unfortunate reality is that in one year we lost a decade of progress against HAIs.” said Ann Marie Pettis, BSN, RN, President of APIC.
These recent jumps in HAIs include:
- a 47% increase in central line-associated bloodstream infections
- a 44.8% increase in ventilator-associated infections
- a 33.8% increase in MRSA infections
- and an 18.8% increase in catheter-associated UTIs
Room Contamination Increases HAI Rates
Pathogens are present on all exposed surfaces and the air, and some can survive and regenerate for quite some time. Pathogen sources include patients, visitors, wheelchairs, tools, shoes, and other elements of the patients’ rooms that are not consistently or effectively disinfected. For example, SARS-CoV-2 has been found to last 3–17 days, E. coli 16 months, MRSA 7 months, and VRE up to 4 months.It’s not surprising: data supports that in a high microbial load environment, patients have more chances of encountering pathogens that can cause infections. As a result, a decrease in room contamination was associated with a decrease in related patient infections.
Shoes as a Vector for Pathogen Transmission
Think about it: When was the last time you washed or sanitized the soles of your shoes? A study at the University of South Florida at a Tampa hospital showed over 75% of people carry harmful pathogenic microorganisms on the soles of their shoes. A University of Arizona study by Charles Gerba, Professor of Virology, found:
- There are about 421,000 units of bacteria on a single pair of shoes.
- Fecal bacteria on 96% of the shoes.
- Bacteria found on the shoes included Escherichia coli, known to cause intestinal and urinary tract infections, meningitis, and diarrheal disease; Klebsiella pneumonia, a common source for wound and bloodstream infections as well as pneumonia; and Serratia ficaria, a rare cause of infections in the respiratory tract and wounds.
- The transfer of bacteria from the shoe to the floor is between 90% to 99% with every step.
Compounding the threat, individual pathogenic cells can double every 20 minutes; and within only 7 hours, 1 single pathogen unit can reproduce to 1 million units.
Microorganisms on the floors are spread to hands, high-touch areas, and redistributed into the air.
A 2020 study, Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China revealed concerning patterns of spread of SARS-CoV-2 in a hospital and concludes, “The rate of positivity was relatively high for floor swab samples (ICU7/10, 70%; GW 2/13, 15.4%), perhaps because of gravity and airflow causing most virus droplets to float to the ground. In addition, as medical staff walks around the ward, the virus can be tracked all over the floor, as indicated by the 100% rate of positivity from the floor in the pharmacy, where there were no patients.”
Yet another study which was published in Infection Control and Hospital Epidemiology in 2016 by Koganti, Donskey et al: Evaluation of Hospital Floors as a Potential Source of Pathogen Dissemination Using a Nonpathogenic Virus as a Surrogate Marker concludes, “We demonstrated that a nonpathogenic virus inoculated onto floors in hospital rooms disseminated rapidly to the hands of patients and to high-touch surfaces inside and outside the room.”
Ultraviolet (UV) Light and Ozone
Let’s talk first about Ultraviolet Light (UV).Research was initiated on the use of UV to kill microorganisms in 1845. By 1877, there was proof that ultraviolet light could destroy microorganisms. Researchers Downes and Blunt observed that exposing test tubes to sunlight prevented the growth of microbes inside a test tube and that with longer exposure times to sunlight the test tubes remained free of microbial growth.
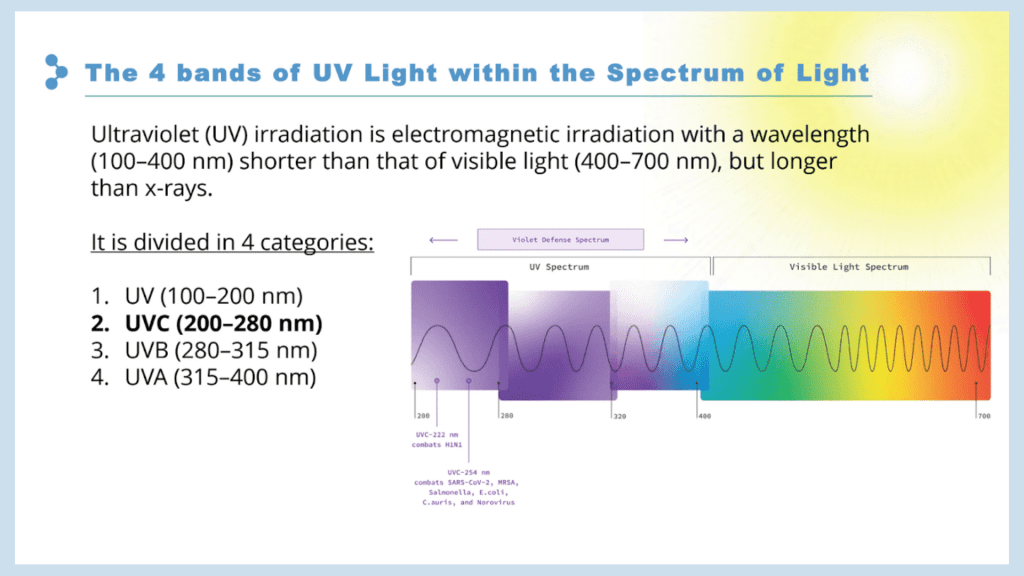
UV radiation is classified by wavelength (the distance between the peaks in a series of waves) which is measured in nanometers. UV-A rays have the longest wavelength at 315–400nm, followed by UV-B (280–315nm), UV-C (200–280nm -peak germicidal wavelength), and finally UV, with the shortest wavelengths of 100–200nm. Specifically, 254nm and 262nm are the optimum wavelengths for disinfection; falling into the UV-C category.
How does UV-C light disinfect?
UV-C radiation kills or inactivates microbes. Proteins, DNA, and RNA in the microbes absorb the UV-C light, rupturing their cell walls. When the DNA or RNA absorbs the radiation, they are inactivated, meaning the microbe is unable to replicate and spread disease. The intensity of UV-C radiation and the exposure time influence how effective the disinfection process is. UV-C damages and can destroy cells because of the accumulation of DNA/RNA damage it causes over the time of exposure.
What is Ozone (O3) and how does it function as a disinfectant?
In Berlin in 1840, the first ozone generator as a disinfection mechanism was manufactured by Von Siemens. It wasn’t until 1893 that the first disinfection application was implemented in the Netherlands for water purification. Nice, France became known as the birthplace of Ozone for Drinking Water Treatment in 1906 after being studied and adopted by French scientists there.
Ozone (O3) is a powerful oxidizing agent and 300x more powerful disinfectant than chlorine bleach. It is a gas made up of 3 oxygen atoms with one strong double bond and one weak single bond. This 3rd oxygen atom with a weak bond breaks off the O3 molecule and attaches to the cell wall of the microorganism, causing the wall to rupture and the DNA/RNA to denature; and has the ability to crack the capsid of a microbe’s outer cell wall.
Specifically, O3 damages the membranes of the enveloped viruses through the peroxidation of phospholipids and by generating numerous reactive oxygen species (ROS) capable of damaging other viral macromolecules. The intensity and exposure time of ozone influences how effective the disinfection process is.
Ozone has been proven to be highly effective at killing bacteria, fungi, and molds, and inactivating viruses. It is more effective against enveloped viruses (like SARS-CoV-2, Influenza, and Hepatitis B and C) than naked/non-enveloped viruses such as Norovirus, Rhinovirus, and Poliovirus.
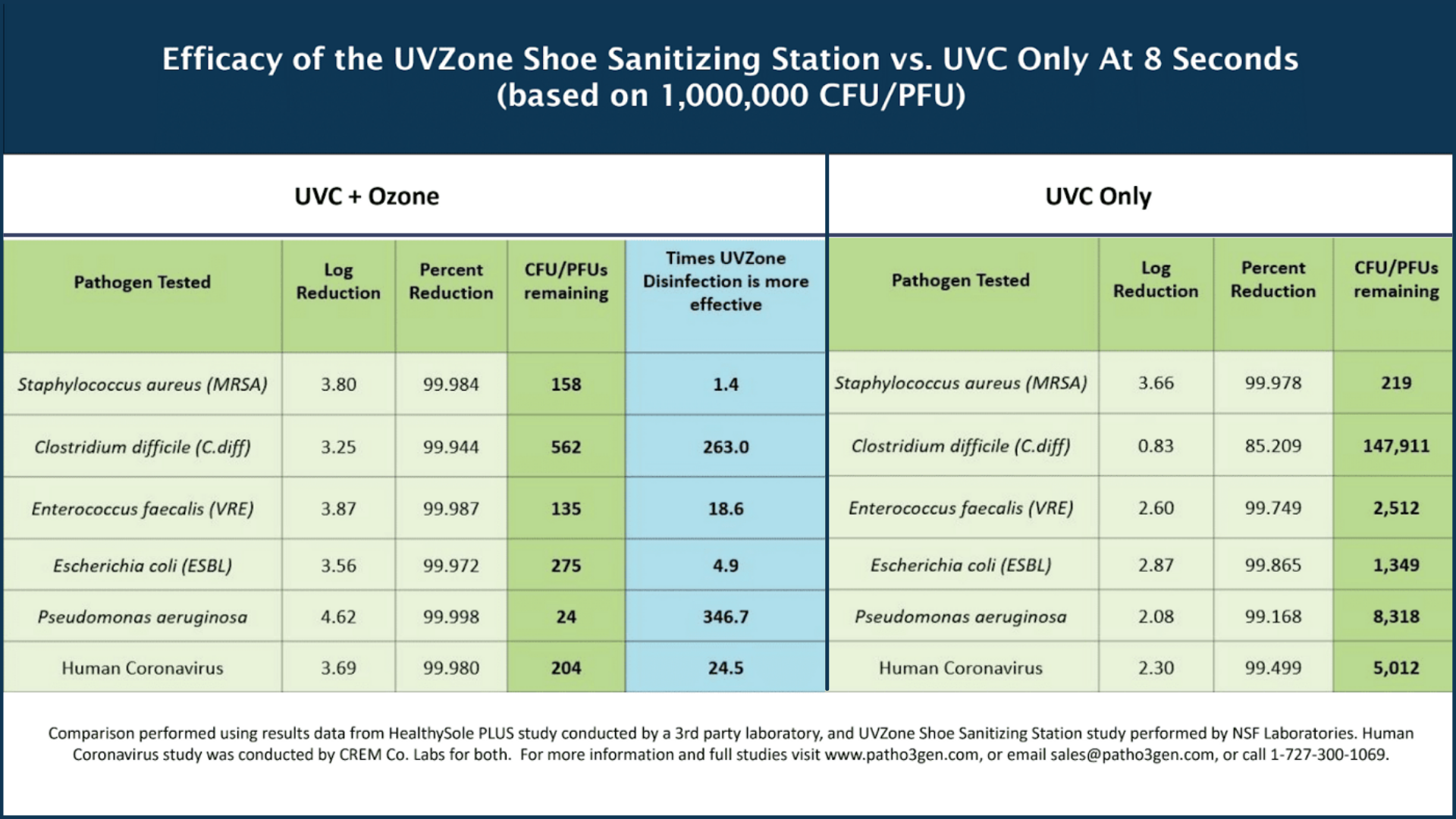
PathO3Gen Solutions has developed the first disinfection technology that combines the power of Ozone (O3) and UV-C light and implements this power in a shoe sanitizing station. Ozone+UV-C is proven to be on average 110x more effective than UV-C light alone in 8 (eight) seconds and destroys up to 99.999% of pathogens on shoe soles in 10 (ten) seconds. The shoe sanitizing stations require no additional staff and provide a safe and effective way to prevent pathogens from entering a facility on shoe soles, 24–7.
Let’s compare other Current Common Practices for floor and shoe sanitizing (Shoe sanitizer data below is based on PathO3Gen Solutions UVZone technology):

TO SUMMARIZE
Shoe Covers: Not Effective
According to a study in the Pakistan Journal of Medical Science, “Not only the use of shoe covers has no benefit regarding the control of infections in the critical care area but also the rates of infection were more. This was probably due to the fact that individuals while putting on the shoe covers… contaminated their hands and thus further transmitted the infection.” Conclusion: Use of shoe covers in the critical care area is not helpful in preventing infections of common ICU pathogens and reducing the length of stay in ICU patients; nor has it decreased the mortality.”
Considerations for Floor Cleaners/Mopping Protocols:
- The 1-Bucket Protocol: The disinfection solution quickly becomes loaded with contaminants mopped up from the floor, then wrung/rinsed into the bucket.
- The 2-Bucket Protocol: Better, but not optimal.
- The 3-Bucket Protocol: This is the industry best practice as it minimizes the disinfectant solution from being contaminated. However, it takes longer, requires more cleaning solution, and is more expensive.
The Benefits of UV-C + Ozone (O3) Disinfection Technology
The combination of Ozone and UV-C light patented by PathO3Gen Solutions and used in the UVZone shoe sanitizing stations provides an easy-to-integrate layer of protection against the spread pathogenic microorganisms. The units plug into a standard outlet, require no chemical use, and are safe to use around people without disrupting workflow. They provide a high level of efficacy, inactivating up to 99.999% of common microbes including E. coli, Listeria, MRSA, C. diff, Candida Auris, and Klebsiella Pneumoniae (as well as leaving zero coronavirus residue) on footwear in only 10 (ten) seconds.
When choosing how to address the disinfection of shoes and floors to create cleaner, safer indoor environments, the efficacy, safety, and ease of use of the UVZone Shoe Sanitizing Stations to disinfect footwear and reduce overall bioburden make it a clear choice for the Sterile Processing Department and Operating Room.